This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.
UnitedHealth Group shares tumbled Friday on a report that the U.S. Department of Justice has started an investigation into the health care giant's Medicare billing practices.
The Wall Street Journal said federal officials have launched a civil fraud investigation into how the company records diagnoses that lead to extra payments for its Medicare Advantage, or MA, plans. Those are privately run versions of the government's Medicare coverage program mostly for people ages 65 and over.
The paper, citing anonymous sources, said the probe focused on billing practices in recent months.
UnitedHealth said it wasn't aware of the start of any new activity as the paper reported. It criticized the Journal's report and said in a statement posted on its website, "Any suggestion that our practices are fraudulent is outrageous and false."

The company's UnitedHealthcare business covers more than 7.8 million people as the nation's largest provider of Medicare Advantage plans. The business has been under pressure in recent quarters due to rising care use and rate cuts.
The Journal's report "adds to a growing worry that expanded oversight around the insurers, particularly in the MA program, could pressure business practices, earnings, and investor sentiment," Leerink Partners analyst Whit Mayo said in a research note.
Shares of the Minnetonka, Minnesota, company fell more than 6% Friday. Shares of other prominent Medicare Advantage insurers like Humana slipped while broader indexes also fell.
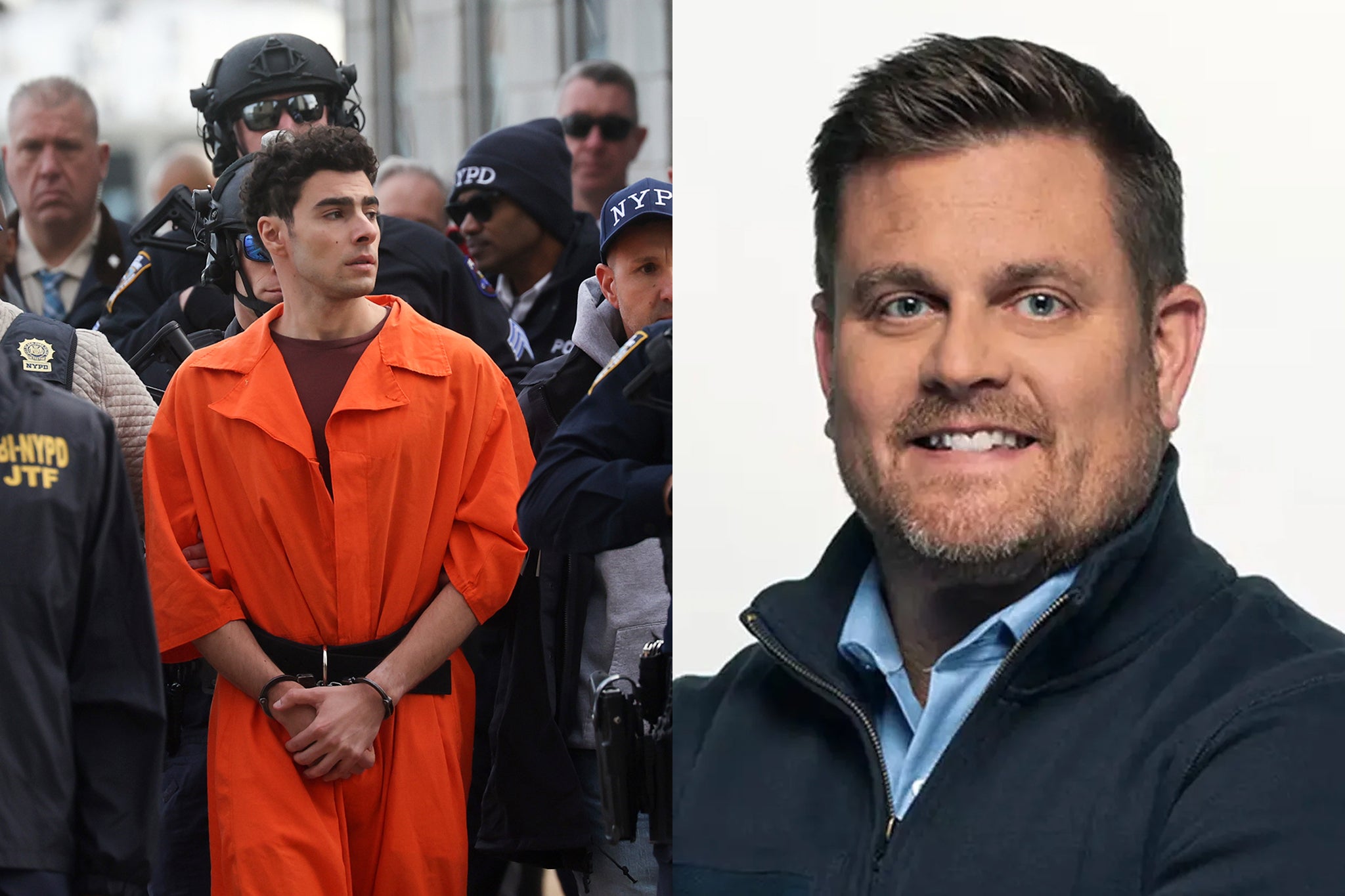
UnitedHealth Group Inc. stock has been in a rut since early December, when UnitedHealthcare CEO Brian Thompson was fatally shot in midtown Manhattan on his way to the company's annual investor meeting. A 26-year-old suspect, Luigi Mangione, who led authorities on a five-day manhunt, was in court Friday for the first time since his December arraignment on state murder and terror charges.
Company shares shed more than $100 in value in the weeks following Thompson's death, as the shooting gave rise to an outpouring of grievances about insurance companies.


 Africana55 Radio
Africana55 Radio 
